In Emphysema, the alveolar air sacs, which are thin walled air space at the end of the airway where Oxygen and Carbon dioxide are exchanged, become damage or destroyed.
The alveoli permanently enlarge and loss elasticity cause difficulty with exhaling, which depends heavily on the ability of lungs to recoil like elastic bands.
Emphysema is lumped under the umbrella of COPD along with Chronic bronchitis. They two differ in that, Chronic bronchitis is defined by clinical features like the productive cough and whereas Emphysema is defined by structural changes, mainly enlargement of air sacs. They almost co-exist, probably because they share the same major cause—Smoking.
With COPD, the airway become obstructed. The lungs don’t empty properly and that leaves air trapped inside the lungs. For that reason, the maximum amount of air people with COPD can breath out in a single breath known as FVC or Forced Vital Capacity is lower.
Emphysema is a form of COPD, that based on structural changes in lungs, specifically a destination of alveoli. Normally, oxygen come in and carbon dioxide go out but when lung tissue is exposed to irritants like Cigarette smoke, it triggers an inflammatory reaction that upset the delicate alveolar walls and affects the flow of gases. Inflammatory reactions attract various immune cells which releases inflammatory chemicals like leukotriene B4, TNF alpha and Proteases. Proteases like Elastases and Collagenases break down structural protein in the connective tissue layers like Elastin and Collagen, which is a protein that gives tissue Elasticity and this leads to problems seem in Emphysema.
In healthy lungs, during exhalation, air whizeus through the airway with high velocity creating a low pressure environment in airway. This is due to Bernoulli’s Principle, where as a fluid–air moves at high velocity, must have low pressure. This low pressure tends to pull the tiny airway inwards. Strong healthy airway wall full of Elastin can withstand that pressure and don’t collapse. They hold the airway open and allow the air to fully escape during exhalation.
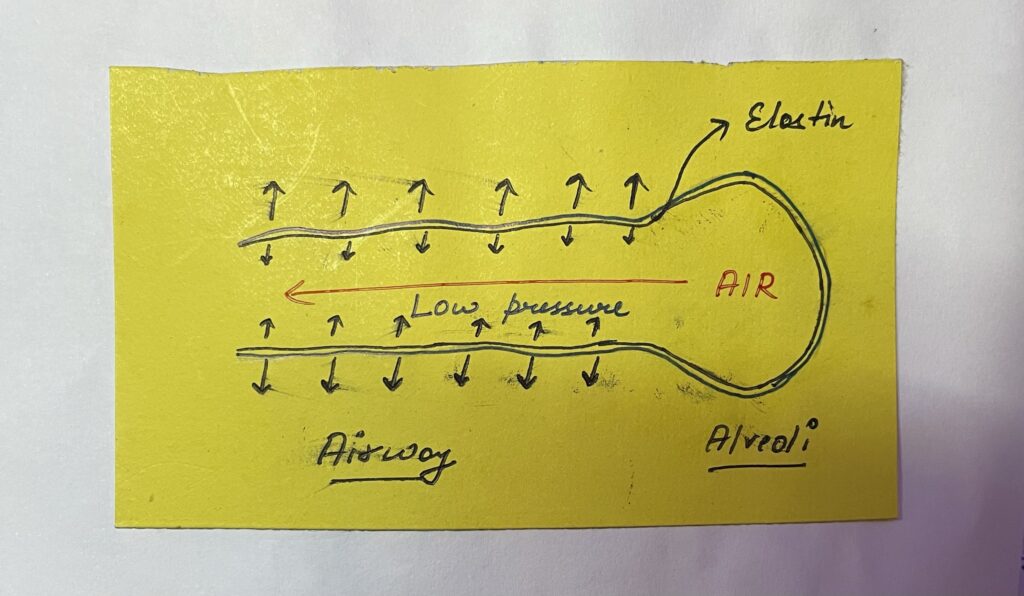
With Emphysema, that Elastin lost, which means the airway walls are weak and that low pressure system to pull the walls inwards and collapse during exhalation. This ultimately leads to air trapping because the collapsed airway traps a tiny bit of air, distal to the point of collapse.

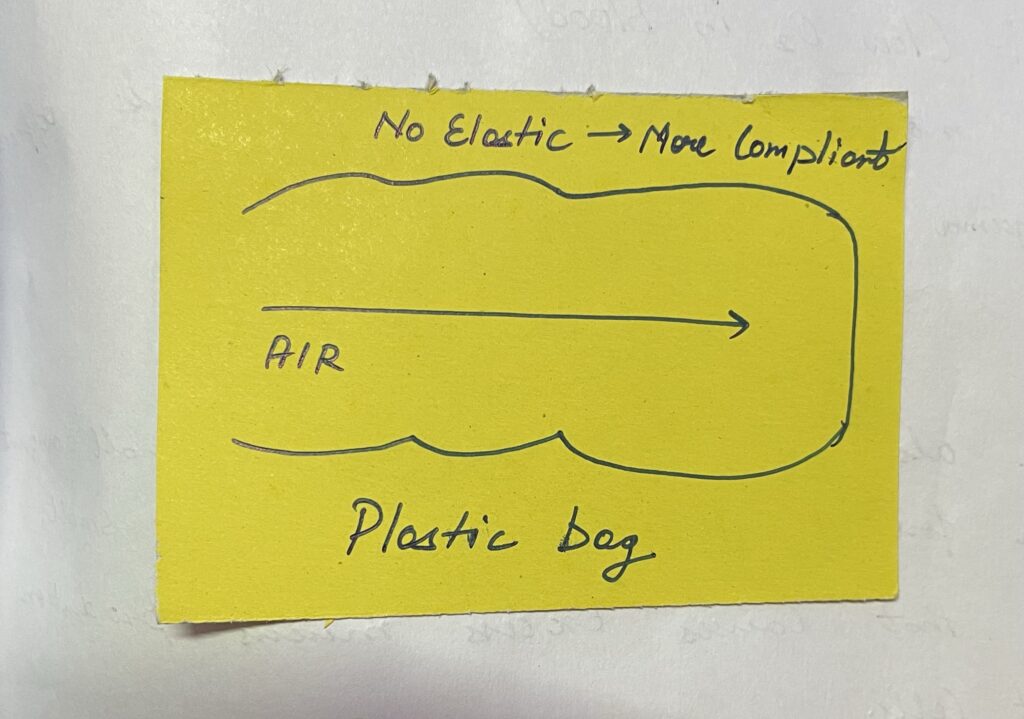
Also, this loss of elastin makes the lungs more compliant, meaning that when air blows into them, they easily expand and then hold onto that air instead of expelling it during exhalation, so lungs start to looks like large Plastic bags.
Symptoms:-
1) Dyspnea (Shortness of breath) – To help counteract this, people sometimes exhale slowly through pursed lips, which increases pressure inside the airway and preventing them from collapsing as easily. This way of breathing explains the nickname ‘Pink Puffer’ since individuals are able to oxygenated their blood but have to purse lips to do so.
2) Weight loss – All of this constant energy spend on breathing can even cause weight loss.
3) Hypoxemia (low oxygen in blood) – Over time more and more lung tissue is affected, thus emphysema lead to hypoxemia.
4) Cough – There can also be cough with a small amount of sputum from inflammation in the small bronchioles that causes excess mucus production via goblet cells.
5) Barrel-shaped chest – Over time, air trapping and hyperinflation of the lungs can cause individual to develop a barrel-shaped chest. On X-ray, individual might have increased AP-Diameter, flattened diaphragm and increase lung field lucency.
Chronic bronchitis, in which bronchitis means inflammation of the bronchial tube in lungs and chronic because it causes a productive cough – which means produce mucus for at-least 3 months each years.
Chronic bronchitis or CB is a type of COPD, that’s diagnosed based on clinical symptoms, specifically coughing up a lot of mucus.
Why does it happen?
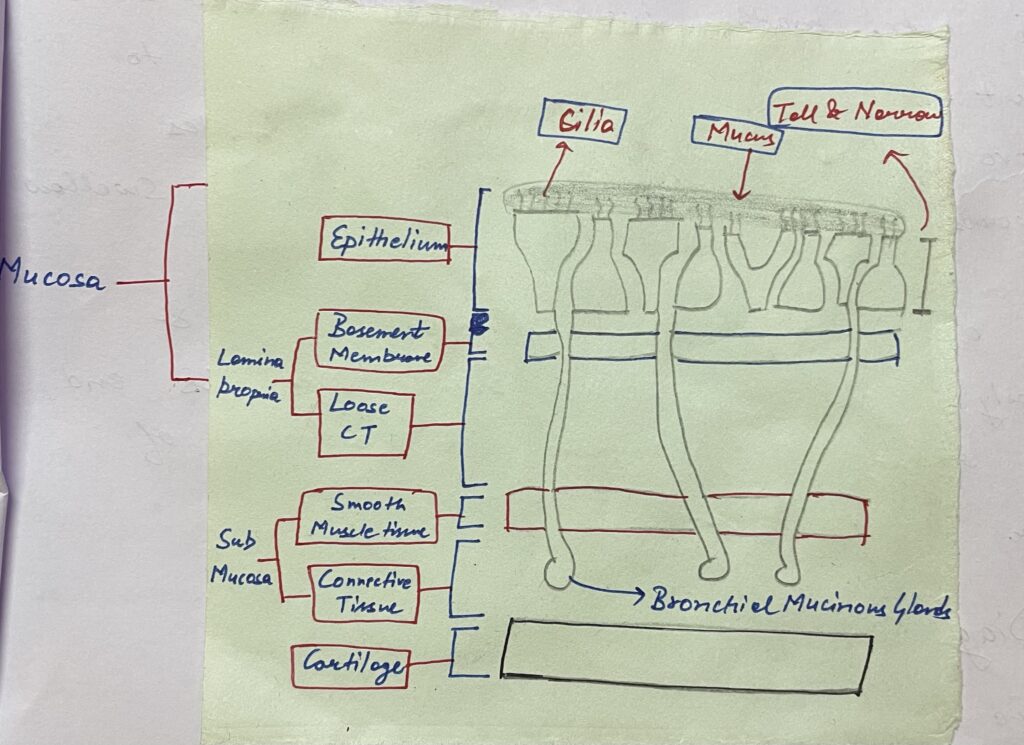
In lungs, the wall of normal airway have a couple of layers to think about. Lining the lumen of airway we got the epithelium, composed of ciliated pseudostratified columnar epithelial cells. This layer also contains occasional goblet cells, which makes some of the mucus that lines the airway. Going deeper past that layer we got the basement membrane and loose connective tissue, called the lamina propria which together with the epithelium makes up the mucosa. Beyond mucosa, there is smooth miscle followed by more connective tissue and together these two layers makes up the submucosa and this is where the bronchial mucinous gland live. These are the gland that secrete the majority of the mucus into the lumen of the bronchi, helping to catch and filter out particles and pathogens.
People with smoke, expose their airway to all sorts of irritants and chemicals. Whatever the irritants are, their effect is to stimulate hypertrophy and hyperplasia of the mucinous gland in the main bronchi, as well as the goblet cells in the smaller airways. The bronchioles which increases mucus production in both location. Since the bronchioles are smaller, even a slight increase in mucus can lead to airway obstruction, so this contributes to the majority of the air trapping. To make matter worse, smoking makes cilia short and less mobile, making it harder to move mucus up and out of bronchioles towards the back of the throat to get swallow. As a result, having too much mucus and poorly functioning cilia, people with CB end up relying on coughing to get rid of their mucus plugs.
Signs & Symptoms:-
1) Wheeze – All the mucus in lungs causes people with CB to wheeze due to narrowing of the passage available for air to move in and out.
2) Crackles (Rales) – Caused by popping open of small airways.
3) Hypoxemia – Low oxygen in blood.
4) Hypercapnea – Increase carbon dioxide in blood because mucus plugs in the airway, block air flow.
Increased carbon dioxide level in blood can get so bad that some people develop cynosis, which is a blue discolouration of the skin and that is why people with CB is referred to as ‘Blue Bloaters’.

